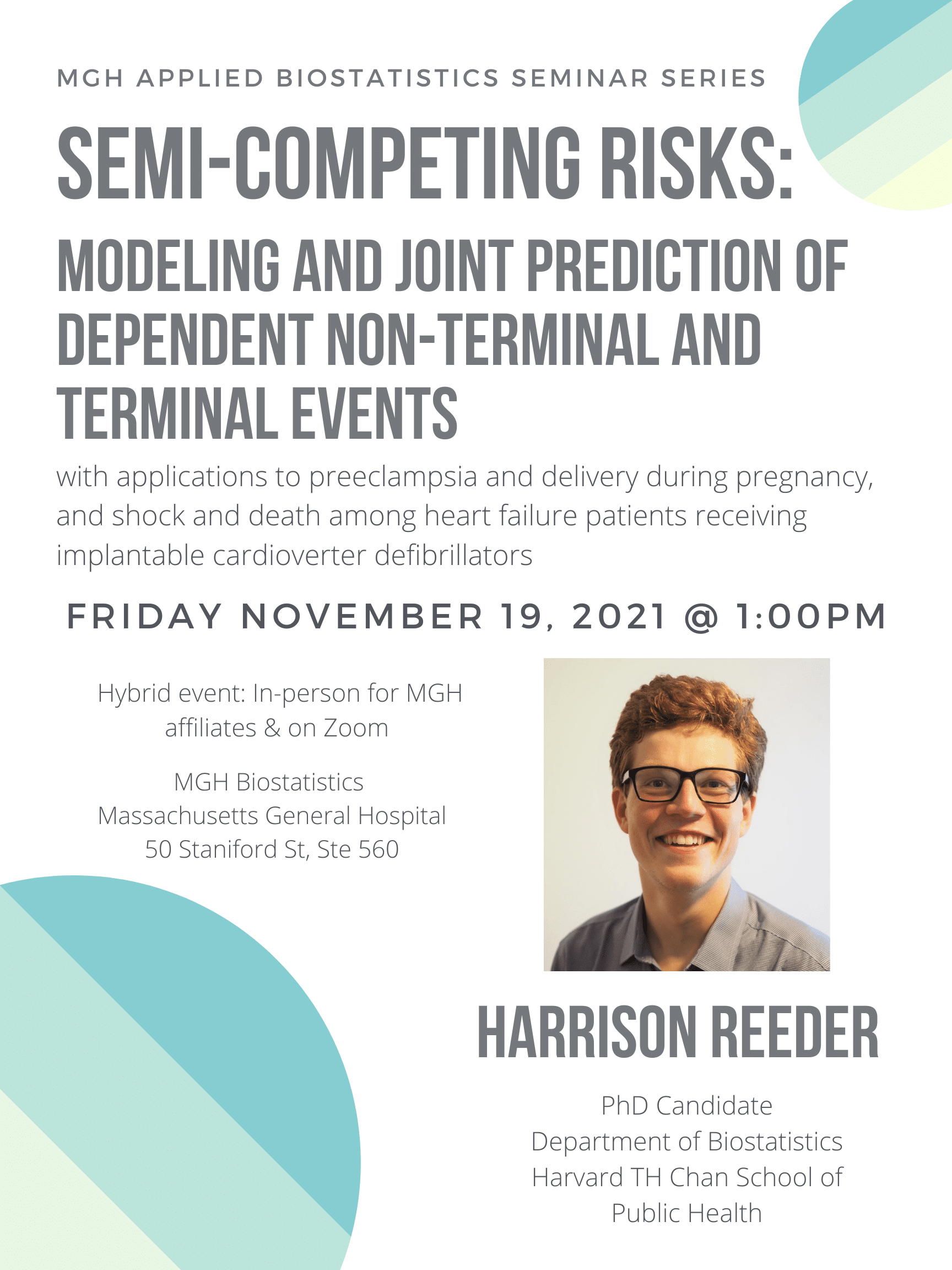
Please join us for the next installment of the MGH Biostatistics Applied Biostatistics Seminar Series, a new seminar series designed to introduce researchers to intermediate topics that are highly relevant to clinical biostatistical research. Presenters will introduce us to their area of expertise and motivate the use of these methods with concrete clinical examples.
The essential role of early phase clinical trials in oncology: design and interpretation
Thursday May 19, 2022, 12:00-1:00pm
Hybrid event: In-person at 50 Staniford St, Ste 560 & on Zoom (https://partners.zoom.us/j/82088584012 )
Speaker: Alexia Iasonos, PhD, Attending Biostatistician, Director, Clinical Research Development, Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York.
Abstract: The specific aims and overall purpose of Phase I clinical trials in oncology have undergone substantial changes over the last several years. The trials originally had a single objective of showing adequate tolerance of an investigational agent or regimen in a heterogeneous patient population. The last several years have seen this single objective evolve into an ambitious set of objectives: to identify the most effective dose of a single agent or combination of agents, the right treatment schedule, and the right patient population in terms of the likelihood of antitumor activity. In this talk, I will provide a broad overview of how the objectives, design, and interpretation of early phase trials have evolved and how the inclusion of dose-expansion cohorts has changed the landscape of early drug development. I will present two recent methodological advancements in this field that aim to correct the bias that can result from errors in toxicity attribution and the bias that can result when the administered dose differs from the assigned dose, which can occur in Phase I trials of CAR T therapy.
This will be a hybrid in-person and virtual event. Dr. Iasonos will be joining us in person for this presentation. Please contact tthaweethai@mgh.harvard.edu with any questions.